Major Depressive Disorder (MDD) is one of the most common mental illnesses in the world, affecting an individual’s physical, cognitive, and social functioning.
What is Major Depressive Disorder (MDD)?
It is important to recognize that depression is different from normal mood fluctuations and short-lived emotions in response to stressors and challenges of everyday life. If an individual is diagnosed with MDD, the manifestations of the low moods are much more intense and persistent, affecting their thoughts, feelings, and behavior (American Psychiatric Association, 2013). Leading to a negative impact on that individual’s physical, cognitive, and social functioning (Huang, 2017). The effects of MDD are specifically more severe and impactful on parents, who have so many obligatory responsibilities with their children, spouse, work, and their own parents. They are at a point in life where multiple stressors are presented daily. Left untreated, MDD is more likely to become chronic, recurrent, and intense, which not only increases the risk of morbidity but also mortality (Kang, 2015).
Effect of MDD on Other Family Members
As a parent, it would not only affect that individual alone, but also all of those around them, specifically their own family. Depression in one family member correlates to an increased incidence of psychopathology and physical morbidity in other family members (Sobieraj, 1998). In this study, Duke University Illness Severity Scores (ISS) was used to assess the burden experienced by two groups: one with an index family member being diagnosed with depression and the other without. Over 11 months, the depression families exhibit a cumulative incidence of depression of 8.9%, in comparison to 1.4% in the Family Practice Unit altogether. Moreover, members of depression families show significant higher ISS than the comparison families (Sobieraj et al., 1998). In conclusion, MDD in either parent can negatively impact parenting quality, increasing the risk of their children developing physical, mental, behavioral, and social problems ((National Research Council and Institute of Medicine, 2009).
Prevalence
Cases of depressive disorder (million) by WHO Region
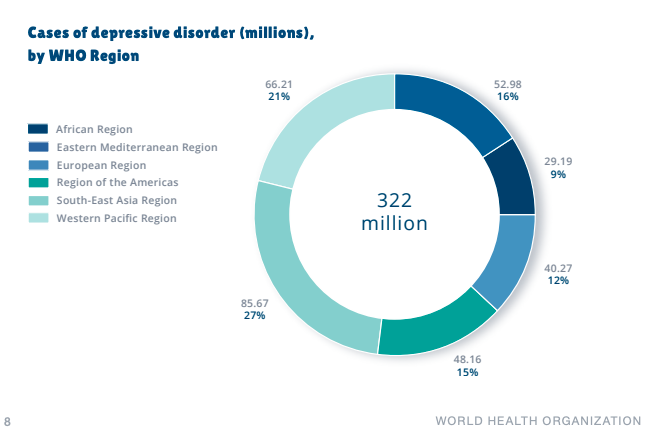
In 2015, the World Health Organization (WHO) reported that depression affects more than 300 million people (see Figure above), estimated to be 4.4% of the global population, in which more women (5.1%) are affected than men (3.6%) (World Health Organization, 2017). WHO estimated that depression will be the number one health concern in both the developed and developing nations by 2030. Although varied effective treatments for mental disorders exist, between 76% and 85% of people in low- and middle-income countries receive no treatment for their disorder (Depression, 2020). Some common barriers to effective treatment in those regions
include lack of resources and trained health professionals, the social stigma about mental disorders, and inaccurate diagnosis. (Depression, 2020). Often, people with depressive symptoms are not correctly diagnosed (both over- and under-diagnosed) and are not properly provided with good prognoses and interventions.
Diagnosis
American Psychiatric Association defined mental disorder in DSM-V as a behavioral, psychological or pattern that occurs in an individual, reflecting an underlying psychobiological dysfunction, leading to clinically significant disability. It must not merely be an expectable response to common stressors and losses or a culturally sanctioned response to a certain event.
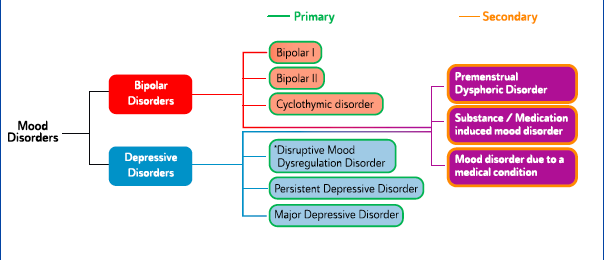
MDD falls under Mood Disorders of the Mental Disorders umbrella (see figure below)
In order to meet the diagnostic criteria by DSM-V, an individual must exhibit at least five of the nine symptoms, in which one of the first two symptoms must be present for most of the day during the same two week period and represent a change from previous functioning (American
Psychiatric Association, 2013):
- Depressed mood
- Loss of interest or pleasure in all or most hobbies and activities
- Increase in appetite, weight gain, or decrease in appetite, weight loss
- Insomnia, early-morning awakening or excessive sleeping
- Restlessness/agitation or slowness in movement
- Decreased energy, fatigue
- Feelings of worthlessness or excessive/inappropriate guilt
- Reduced concentration, memory, and indecisiveness
- Recurrent thoughts of death or suicide, suicide attempts
Comorbidities
WHO predicted that depression will be the leading cause of disease burden in 2030, which might indicate an anticipated burden of depression in the context of physical disorders. A 1-year prevalence study among 30,801 adults in the US discovered that patients were three times more likely to get depressed when suffering from chronic medical diseases in comparison to healthy controls (Kang et al., 2015). Furthermore, another study among 245,400 patients from 60 countries carried out by WHO identified that 9.3% to 18% of subjects with a single physical disorder had depression, whereas only 3.2% of subjects without a physical disorder had depression. Furthermore, nearly a quarter (23%) of patients with two or more physical conditions suffered from depression.” (Kang et al., 2015).
Depression on Parenting Outcomes
Parental depression had a detrimental impact on parenting, family functioning, parent-child relationships, and children’s physical, social, and behavioral health, and cognitive functioning (Huang et al., 2017). Empirical evidence from comprehensive investigations supported that depressed mothers are more likely to exhibit decreased sensitivity with children, lower responsiveness, more intrusive and controlling parenting, poorer monitoring of child health needs, and experience poorer quality of parent-child interactions and lowered parental self-efficacy (Huang et al., 2017). Although less is known about parenting in fathers with depression, many studies are consistent with the findings about mothers. (National Research Council and Institute of Medicine, 2009).
Parent Depression and Children Outcomes
Parental depression may contribute to their children potentially having poor emotion regulation abilities, lack of adaptive skills, and increased mental and physical health problems (Huang et al., 2017). Families with one or more depressed parents usually have additional risk factors affecting children, such as substance use disorders, poverty, exposure to violence, minority status, cultural and linguistic isolation, and marital conflicts (National Research Council and Institute of Medicine, 2009).
Treatment for Depression
Management of major depressive disorder.

As seen in image above, there are several methods for the management of MDD. Ultimately, it can be broken down into two main methods: Pharmacological (antidepressants) and nonpharmacological (psychological therapy, psychosocial interventions, and lifestyle changes). Adoption of regular exercise is recommended as the very first step in the management of MDD, as part of lifestyle changes. It is sometimes difficult for people with MDD to adopt regular exercise habits, as depression often affects people’s sleep and diet. When somebody’s sleep and diet are affected, it may lead to a loss of energy, mood, and a decline in physical ability. The lack of movement may worsen the quality of sleep and diet. Therefore, not being active may lead to a vicious cycle that affects the person’s physical and mental health within their work, social, and personal lives. Breaking out of the vicious cycle by adopting active habits can be incredibly beneficial.
Efficacy of Exercise as a Treatment for Depression
Exercise was found to be an effective intervention for depression, evidenced by a meta-analysis of 23 randomized controlled trials (RCTs) and 977 participants. Exercise yielded a significant effect size when compared to no intervention and usual care. The effects of exercise when compared to psychological treatments or antidepressant medication were small and not significant. Exercise as an adjunct to antidepressant medication yielded a moderate effect that trended toward significance (Kvam et al., 2016).
However, it is important to acknowledge that patient adherence may be a major setback to the efficacy of exercise as a viable treatment. Adopting exercise habits is perceived as more demanding for a person suffering with depression in comparison to other treatment methods, such as taking antidepressants. Nonetheless, exercise has multifaceted psychological and physiological benefits (see figure below) on the treatment of depression and is inexpensive, safe, and has no side effects (Ranjbar et al., 2015)

Exercise Recommendation
The Characteristics of an Exercise Program that will Maximize the Anti-depressive Properties
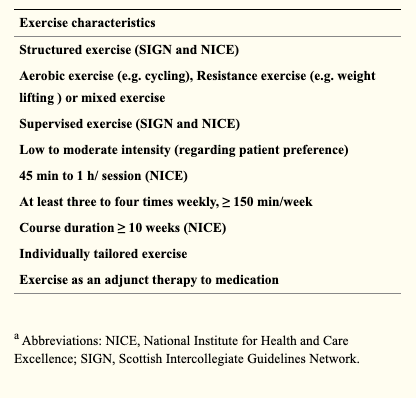
After a long debate regarding the best type of exercise, both aerobic and anaerobic exercises seem to be equally effective in decreasing depressive symptoms. Considering all factors from most recent studies:
It is recommended that moderate intensity training (70% of one repetition max) and 30 minutes on most days, if not all, of the week in adults and twice a week in elderly people is the best condition to achieve immediate, large, and enduring anti-depressants effects.
Ranjbar et al., 2015
Also, it is suggested that the greater benefits are seen when maintaining this exercise recommendation for at least 10 weeks, and preferably, more than 15 weeks. As mentioned before, the context of exercise (where, when and with whom) may be even more important to discuss with your patient than the prescription itself (type, intensity, frequency), as the major threat to exercise treatment is patient adherence. To achieve maximal benefits, a multidisciplinary team of health care specialists (e.g. general practitioners, psychologists, accredited exercise physiologists, etc.) must work together to recommend an exercise program that is patient-centered, safe, progressive, fun, rewarding, efficient, and realistic (Ranjbar et al., 2015).
Final Considerations
Untreated MDD could lead to multiple vicious cycles. At a personal level, people suffering with depression may already be suffering from the complex negative effects of psychological, social, and biological factors. If a parent is suffering with depression, it may increase the incidence of depression and physical illness in their family members (Sobieraj, 1998). Specifically, it would affect their children, creating an intergenerational vicious cycle. Nonetheless, there are multiple effective treatments for MDD if a person seeks them, one of which is exercise, which is comparable to psychotherapy and antidepressants due to its multifaceted benefits on biological and psychosocial factors. It could also be a viable adjunct treatment along with antidepressants (Kvam, 2016).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Depression. (2020, January 30). Retrieved from https://www.who.int/news-room/factsheets/ detail/depression
- Huang, K. Y., Abura, G., Theise, R., & Nakigudde, J. (2017). Parental Depression and Associations with Parenting and Children’s Physical and Mental Health in a Sub-Saharan African Setting. Child psychiatry and human development, 48(4), 5178527. https://doi.org/10.1007/s10578-016-0679-7
- Kang, H. J., Kim, S. Y., Bae, K. Y., Kim, S. W., Shin, I. S., Yoon, J. S., & Kim, J. M. (2015). Comorbidity of depression with physical disorders: research and clinical implications. Chonnam medical journal, 51(1), 8-18. https://doi.org/10.4068/cmj.2015.51.1.8
- Kvam, S., Kleppe, C. L., Nordhus, I. H., & Hovland, A. (2016). Exercise as a treatment for depression: A meta-analysis. Journal of affective disorders, 202, 67-86. https://doi.org/10.1016/j.jad.2016.03.063
- Malhi, G., Basset, D., Boyce, P., Bryant, R., Fitzgerald, P., Fritz, K., Hopwood, M., Lyndon, B., Mulder, R., Murray, G., Porter, R., & Singh, A. (2015). Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders.
- National Research Council (US) and Institute of Medicine (US) Committee on Depression, Parenting Practices, and the Healthy Development of Children; England MJ, Sim LJ, editors. Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention. Washington (DC): National Academies Press (US); 2009.
- Ranjbar, E., Memari, A. H., Hafizi, S., Shayestehfar, M., Mirfazeli, F. S., & Eshghi, M. A. (2015). Depression and Exercise: A Clinical Review and Management Guideline. Asian journal of sports medicine, 6(2), e24055. https://doi.org/10.5812/asjsm.6(2)2015.24055
- Sobieraj, M., Williams, J., Marley, J., & Ryan, P. (1998). The impact of depression on the physical health of family members. The British journal of general practice: the journal of the Royal College of General Practitioners, 48(435), 1653-1655.
- World Health Organization. (2017). Depression and Other Common Mental Disorders: Global Health Estimates. Geneva. Licence: CC BY-NC-SA 3.0 IGO.





This Post Has One Comment
Pingback: Soy Myth Debunked: A Healthy Source of Protein - Orbit
Comments are closed.