To improve population health and achieve health equity, it is important to understand the underlying factors that influence health outcomes. There are a variety of determinants that influence health. In this article we discuss the social and economic factors that affect health outcomes, known as the social determinants of health.
What are Social Determinants of Health? (5, 7, 9, 10)
Health is influenced by numerous factors. Among many, these may include individual factors (e.g., age, sex, genetics), behavioural factors (e.g., smoking, physical activity, eating habits), or social factors. The World Health Organization defines the social determinants of health as:
“The non-medical factors that influence health outcomes. This refers to a set of conditions in which people are born, grow, work, live, and age that shape the conditions of daily life.”
World Health Organization
5 domains That Impact People’s Health
The social determinants of health include 5 domains: 1) social and community networks; 2) socio-economic status; 3) education access and quality; 4) environmental conditions, and 4) health care access and quality.
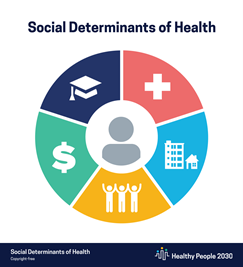
- Social and Community Networks: The relationships people have with their family, friends, co-workers, and community. These relationships influence behaviours, mental health, and physical health.
- Socio-Economic Status: This relates to the social and economic standing of an individual in society, often measured in terms of education, work, occupation, and income.
- Education Access and Quality: A person’s ability to pursue school, to obtain a high school diploma, or to attend higher education. Educational systems provide essential knowledge and skills in language, literacy, health and wellbeing.
- Environmental Conditions: The area in which a person resides. Important aspects within this domain are the quality and availability of housing, food, air, water, access to transportation, and presence or absence of violence and crime.
- Health Care Access and Quality: The connection between an individual’s knowledge of their health, health care services, and accessibility to health care facilities. Issues addressed within this domain include accessibility to health care facilities and professionals, insurance, and health literacy.
How Does This Relate to One’s Quality of Life?(3, 9)
The domains of the social determinants of health greatly impact the health and quality of life of all people in positive or negative ways. Fundamentally, these determinants are shaped by the distribution of money, power, and resources. When people have access to resources (e.g., education, safe housing, transportation, job opportunities, affordable health care, nutritious food, physical activity opportunities), they are more likely to have favourable health outcomes. Conversely, if a person does not have access to the aforementioned resources, they will be more likely to endure negative health outcomes. For example, if a person lives in a polluted neighbourhood, faces discrimination, or does not have access to a grocery story, they will be more likely to face malnourishment, experience chronic stress, or be less willing to go outside due to the air quality.
Just promoting healthy choices won’t eliminate health disparities. Instead, public health organizations and their partners in sectors like education, transportation, and housing need to take action to improve the conditions in people’s environments.
Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion
Shifting The Conversation Beyond Behaviours (11)
Traditionally, the conversation around improving population health has been focused on behavioural factors such as smoking, physical inactivity, nutrition, alcohol, or drug use. Research has certainly shown that physical activity and eating nutritious foods improves people’s well-being on the long-term and short term. Being able to “feel” and attune yourself to what exercise and foods your body needs presents positive health outcomes. That being said, despite the positive outcomes that may result from a behaviour modification (such as eating more nutritious foods or exercising), it would be wrong to assume that exercise or diet alone can determine your health. According to the U.S. Centers for Disease Control and Prevention and other studies and internationally-renown organizations, health behaviours account for less than a quarter of health outcomes in different groups.
So, while behavioural factors might influence your health, social differences will account for most people’s health differences. Living in a polluted neighborhood, fearing crime, experiencing racism, sizism, not having access to stable housing, education, or support networks, are all examples of situations that will trigger chronic stress, impacting one’s general health and wellbeing, more than any lifestyle modification.
Health Equity and Intersectionality(1, 2, 3, 4, 6, 8,12)
Health equity has become an important priority for governments, educational systems, and health care professionals. Achievement of health equity is a collective effort that requires action from all sectors (e.g., education, housing, employment).
Health equity is when everyone has the opportunity to ‘attain their full health potential’ and no one is disadvantaged from achieving this potential because of their social position or other socially determined circumstance.
(Ramirez et al., 2008, p. 6)
Previously in this article, we addressed some important determinants that create unequal and inequitable health statuses across populations. However, we did not mention two of three major factors that contribute to chronic environmental stressors that will put some people more at risk of illness and death than others: Race/ethnicity and gender. The third is socioeconomic status, which we discussed.
Intersectionality
When working to achieve health equity, health professionals must acknowledge the intersecting facets that come to shape that person’s health, notably those people who are disadvantaged because of their social position.
Excluded or marginalized groups have been pushed to society’s margins, with inadequate access to key opportunities. They are economically and/or socially disadvantaged. Examples of historically excluded/marginalized or disadvantaged groups include—but are not limited to—people of color; people living in poverty, particularly across generations; religious minorities; people with physical or mental disabilities; LGBTQ persons; and women.
Braveman et al., 2017, p.6
As we work toward health equity, we cannot lose sight of intersectionality, that is the “multiple systems of oppression that exist at the same time to help explore the framework between co-existing identities.” The term intersectionality was coined by Kimberle Crenshaw (1989).
In Practice: If you are an educator, and have a student that constantly arrives late to school, never wants to take part in physical education, does not have lunch every second day, and creates disruption in your teaching space: How might that student’s social circumstances and intersecting identities result in these behaviours? How might this consideration impact the way you talk to that student and respond to those behaviours?
Summary
Understanding that health is determined by numerous factors, far beyond behaviours, may allow for more people to view people’s health status more comprehensively, and most importantly, with more compassion.
References
- Andermann, A. (2016). Taking action on the social determinants of health in clinical practice: A framework for health professionals. Canadian Medical Association Journal, 188(17-18), E474-E483. https://doi.org/10.1503/cmaj.160177
- Artiga, S., & Hinton, E. (2018). Beyond health care: The role of social determinants in promoting health and health equity. KFF. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
- Bernazzani, S. (2016, May 1). The importance of considering the social determinants of health. American Journal of Managed Care. https://www.ajmc.com/view/the-importance-of-considering-the-social-determinants-of-health
- Brennan Ramirez, L.K., Baker,E.A., Metzler, M. (2008). Promoting health equity: A resource to help communities address social determinants of health. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
- Centers for Disease Control and Prevention. (2021). About social determinants of health (SDOH). https://www.cdc.gov/socialdeterminants/about.html
- Centers for Disease Control and Prevention. (n.d.). NCHHSTP social determinants of health. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html#:~:text=Addressing%20social%20determinants%20of%20health%20is%20a%20primary%20approach%20to,other%20socially%20determined%20circumstance’%E2%80%9D
- Healthy People 2030. (n.d.). Social determinants of health. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- Umberson, D., Montez, J. K. (2011). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51, S54-S66. https://doi.org/10.1177/0022146510383501
- World Health Organization. (n.d.). Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved [date graphic was accessed], from https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- Bacon, L., & Apramor, L. (2014). Body Respect: What Conventional Health Books Get Wrong, Leave Out, and Just Plain Fail to Understand about Weight. BenBella Books
- Braveman P, Arkin E, Orleans T, Proctor D, and Plough A. What Is Health Equity? And What Difference Does a Definition Make?Princeton, NJ: Robert Wood Johnson Foundation, 2017